Research Objectives:
Examine the predictive prevalence of major depressive episodes (MDE), MDE with severe impairment, MDE with alcohol use disorder in relation to sociodemographic disparity and frequency of cannabis use.
Keywords:
marijuana, depression, cannabis, severe role impairment, alcohol use disorder (AUD)
Bio
Dr. Ismatara Reena, Ed.D, MBBS, CHES, serves as an Assistant Professor in the Health Promotion and Wellness Program at the University of Louisiana at Lafayette, USA. Her diverse research portfolio spans underrepresented groups, mental health literacy, social determinants of health, COVID-19’s effects on higher education, and health equity. With a passion for promoting wellness and addressing disparities, she contributes invaluable insights to the field. Dr. Reena’s work underscores her commitment to advancing knowledge and fostering positive change in healthcare and education. Her multidisciplinary approach and dedication to improving health outcomes make her a valuable asset to the academic community and beyond.
Abstract
Youth substance use is a major public health concern. Marijuana and alcohol, the two most common illicit drugs among adolescents are increasing being studied for affective risk. Despite the steady fall of teens substance use since pandemic, teens depressive symptoms elevated, and mental health condition worsened. This study investigates the association between adolescent marijuana use, depression, and alcohol use disorder (AUD) using data from the 2021 National Survey of Drug Use and Health (NSDUH). Descriptive statices and binary logistic regression were used analyse the data.
The findings reveal that adolescent marijuana use is significantly associated with higher odds of lifetime MDE, past-year MDE, past-year MDE with severe role impairment, and past-year MDE with AUD. Female gender and White race followed by Hispanic have statistically higher marijuana consumption. Two out of five adolescent lifetime marijuana user had past year MDE, and 9% had MDE with AUD. A significant portion of adolescents, ranging from 63% to 75%, perceive moderate to heavy marijuana use as lacking substantial risks. A consistent and particular escalating odds is identified between past-year cannabis use frequency and the likelihood of experiencing MDE with co-occurring AUD.
Introduction
Marijuana and alcohol are among the most common form of psychoactive polysubstance use globally particularly among adolescents (Banks et al., 2017; Jones & McCance‐ Katz, 2019). In 2020, nearly 900,000 adolescents had alcohol use disorder and 1.3 million people had marijuana use disorder (Substance Abuse and Mental Health Services Administration [SAMHSA], 2022). Cannabis reforms such as decriminalization, medicalization, and legalization have had varied consequences youth in the United States, including some advantages and detrimental consequences on adolescent mental health (Hammond et al., 2020). Marijuana and alcohol alone or when used together has disproportionate population distribution (McHugh, 2019; Gajos et al., 2021; Pedroni et al., 2021; Siddiqui et al., 2022). Both substances are linked to a wide range of acute and long-term health hazards and repercussions (Aloi et al., 2019; Crocker et al., Marijuana and alcohol are among the most common form of psychoactive polysubstance use globally particularly among adolescents (Banks et al., 2017; Jones & McCance‐ Katz, 2019). In 2020, nearly 900,000 adolescents had alcohol use disorder and 1.3 million people had marijuana use disorder (Substance Abuse and Mental Health Services Administration [SAMHSA], 2022). Cannabis reforms such as decriminalization, medicalization, and legalization have had varied consequences youth in the United States, including some advantages and detrimental consequences on adolescent mental health (Hammond et al., 2020). Marijuana and alcohol alone or when used together has disproportionate population distribution (McHugh, 2019; Gajos et al., 2021; Pedroni et al., 2021; Siddiqui et al., 2022). Both substances are linked to a wide range of acute and long-term health hazards and repercussions (Aloi et al., 2019; Crocker et al., 2021; Pasman et al., 2018; Reece & Hulse, 2020).
Overall, a steady fall of substance use has been noticed among adolescents since the pandemic culmination, yet the upward trajectory of depression prevalence remains same among all demographics (Patalay & Gage, 2019). Higher marijuana consumption attributed to the discourse on cannabis reform can translate into a greater mental healthcare burden (Bodden et al., 2018; Mojtabai et al., 2016; Ssegonja et al., 2019; Twenge, 2020; Zuckermann et al., 2019). Converging evidence of robust literatures indicate the association of cannabis use to depression in adolescents (Chadi et al., 2019; Langlois et al., 2021; Weinberger et al., 2020), however the directionality is not clear. The relationship between cannabis uses and depression has three hypotheses so far: depression preceding cannabis use, cannabis-induced brain changes increasing MDD risk, and confounding factors (Gukasyan & Strain, 2020). In contrast, ample scholarly works have demonstrated the association of risk of depression with alcohol misuse.
However, the results of extensive population-based surveys show that depression brought on by solely drinking alcohol is not extremely prevalent. Studies have revealed that many cases that were initially diagnosed as alcohol-induced depression were later reclassified as independent depression (i.e., not substance caused), as the condition persisted even after a period of abstinence (McHugh, 2019).
Marijuana use can potentially lead to use of other substances including alcohol (Hines et al., 2020; Nugent et al., 2018; Ramlagan et al., 2021). A large number of adolescents in the U.S. are engaged in substance use according to recent national surveys (SAMHSA. 2022). In 2021, The percentage for marijuana vaping in the past month among current marijuana users was highest among adolescents. In 2020, Nearly 900,000 adolescents had alcohol use disorder and 1.3 million people had marijuana use disorder. In addition, 20.1 percent (weighted 5.0 million adolescents) had major depressive episode (MDE), and 14.7 percent (weighted 3.7 million adolescents) had MDE with severe impairment in various roles of life. Among adolescents aged 12 to 17, 2.9 percent (weighted 724,000 people) had both an MDE with severe impairment and an substance use disorder (SUD). Additionally, a concerning prevalence of depression effects like suicidal thoughts, plans, and attempts among adolescents was observed. The estimates are derived from surveying in the subsequent year. This high prevalence raises the concern for outlining the predictors of depression related to substance use.
Although co-use of alcohol and marijuana and its associated risk of moderate depression has been studied several times in several demographics (Claus et al., 2017; Lipperman‐ Kreda et al., 2017; Thompson et al., 2021; White et al., 2019), the impact of cannabis use on MDE with alcohol use disorder (AUD) has not been studied enough. The relevance to identify the sociodemographic disparity is paramount importance to recognise target strata of population. With shifting cannabis legalization in the US, and alcohol being the second most common used substance, it’s crucial to investigate the link between adolescent cannabis use with adolescent with major depressive episodes and with alcohol use disorder and the pattern of population distribution.
The objective of the current study is to examine the predictive prevalence of major depressive episodes (MDE), MDE with severe impairment, MDE with alcohol use disorder in relation to sociodemographic disparity and frequency of cannabis use.
Method
This research employed a secondary data analysis approach, utilising data from the 2021 National Survey of Drug Use and Health (NSDUH). The study included a total of 10,743 adolescent participants aged 12-17, drawn from the NSDUH database. The data were nationally representative of the United States population. The NSDUH conducted multimodal data collections throughout 2021, compiling information from households, non institutionalised group quarters, and civilians on military bases. Data were anonymized and available for public use.
The primary outcome measures were lifetime major depressive episodes (MDE), past year MDE, past year MDE with alcohol use disorder (AUD) and past year MDE with severe role impairment. All outcomes were binary dichotomous variables, with responses categorized as “Yes” or “No.” The NSDUH adapted discrete adolescent depression criteria from the Diagnostic and Statistical Manual of Mental Disorders-5 (American Psychiatric Association, 2013) to define lifetime MDE.
Past year depression was determined for those with lifetime MDE reporting a 2-week or longer period of depression in the past 12 months. Adolescents concurrently reporting alcohol abuse underwent assessments for alcohol use disorder. The Sheehan Disability Scale (Leon et al., 1997) measured the impact of a disorder on adolescents’ life, assessing role functioning in chores, relationships, and social life.
Adolescents were classified as having an MDE with severe impairment if their depression caused severe problems with their ability to do chores at home, do well at work or school, get along with their family or have a social life. Scores ≥7 in any domain indicated MDD with severe role impairment. Independent variable, cannabis use frequency was obtained by classifying past year cannabis use into four categories: non-user, mild user (1-11 days a year), moderate user (12-49 days a year), and heavy user (≥50 days a year) (Gukasyan & Strain, 2020).
Descriptive analysis characterized participant demographics and assessed the prevalence of cannabis use. Binary logistic regression analyses were conducted to predict the probabilities of experiencing lifetime major depressive episode, past year major depressive episode, major depressive episode with severe role impairment, major depressive episode with alcohol use disorder based on sociodemographic factors and cannabis use frequency. Odds ratios (OR) with 95% confidence intervals (CI) quantified the observed associations. All statistical analyses were performed using SPSS version 26.0, with a significance cutoff of 0.05 and a 95% confidence level.
Results
Participants Characteristic
Table 1 presents sociodemographic characteristic of participants (N= 10743, weighted about 25 million adolescents) by marijuana use. Weighted column percents and unweighted n of the total sample adolescents who had lifetime marijuana use across various sociodemographic variables and depression outcomes including severe impairment and alcohol use disorder (AUD).
Most of the adolescent participants with lifetime marijuana use are older adolescents (age 16-17, 63.9%), females (54.7%), non-Hispanic white (51.4%) followed by Hispanic (23.3%), with a total annual family income $50,000 or more (58.1) and are found to be statistically significant with crosstab chi-square analysis. In 2021, nearly 50% of adolescents who used cannabis experienced at least one major depressive episode (MDE) in their lifetime. Additionally, around 40% reported MDEs in the preceding year, with about 31% encountering MDEs associated with severe role impairment, and roughly 9% with co-occurring alcohol use disorder. All the depression outcomes including past year MDE with AUD demonstrated significant associations with marijuana use (p < 0.01).

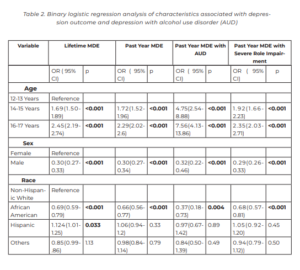
Prediction by sociodemographic variables
The findings of the study (see Table 2) reveal significant associations between various demographic factors and the likelihood of experiencing depression outcomes. For lifetime MDE, adolescents aged 14-15 years exhibited a significantly higher likelihood (OR = 1.69, 95% CI: 1.50- 1.89, p < 0.001), while those aged 16-17 years had an even greater likelihood (OR = 2.45, 95% CI: 2.19-2.74, p < 0.001) compared to the reference group (12-13 years). A similar pattern was observed for past year MDE, with higher odds for both the 14-15 years group (OR = 1.72, 95% CI: 1.52- 1.96, p < 0.001) and the 16-17 years group (OR = 2.29, 95% CI: 2.02-2.6, p < 0.001). Concerning past year MDE with alcohol use disorder, the odds were significantly elevated for adolescents aged 14-15 years (OR = 4.75, 95% CI: 2.54-8.88, p < 0.001) and 16-17 years (OR = 7.56, 95% CI: 4.13-13.86, p < 0.001) compared to the reference group. Similarly, for past year MDE with severe role impairment, both the 14-15 years group (OR = 1.92, 95% CI: 1.66-2.23, p < 0.001) and the 16-17 years group (OR = 2.35, 95% CI: 2.03- 2.71, p < 0.001) displayed significantly higher odds.
For lifetime MDE, males demonstrated a significantly lower likelihood than female (OR = 0.30, 95% CI: 0.27-0.33, p < 0.001), and this pattern persisted for past year MDE (OR = 0.30, 95% CI: 0.27-0.34, p < 0.001). Similarly, for past year MDE with alcohol use disorder, male adolescents exhibited a markedly reduced likelihood (OR = 0.32, 95% CI: 0.22-0.46, p < 0.001), as did for past year MDE with severe role impairment (OR = 0.29, 95% CI: 0.26-0.33, p < 0.001).
In comparison with non-Hispanic white adolescents, the odds of lifetime MDE among African American adolescents were significantly lower (OR = 0.69, 95% CI: 0.59-0.79, p < 0.001), and this pattern persisted for past year MDE (OR = 0.66, 95% CI: 0.56-0.77, p < 0.001) and past year MDE with severe role impairment (OR = 0.68, 95% CI: 0.57-0.81, p < 0.001). However, for past year MDE with alcohol use disorder, the odds were significantly lower only for African American adolescents (OR = 0.37, 95% CI: 0.18-0.73, p = 0.004). In the Hispanic group, the odds of lifetime MDE were slightly higher (OR = 1.124, 95% CI: 1.01-1.25, p = 0.033), but there were no significant associations for past year MDE, past year MDE with alcohol use disorder, or past year MDE with severe role impairment.
For adolescents in families with an income of $20,000- $49,999, the odds of lifetime MDE were slightly elevated (OR = 1.19, 95% CI: 1.02-1.38, p = 0.02) than less than $20,000 group. Although a similar trend was observed for past year MDE, it did not reach statistical significance (OR = 1.12, 95% CI: 0.95-1.31, p = 0.19). There were no significant associations between this income range and past year MDE with alcohol use disorder or past year MDE with severe role impairment. In contrast, families with an income of $50,000 or more did not show any signifcant association with lifetime MDE (OR = 1.10, 95% CI: 0.967-1.258, p = 0.14) or past year MDE (OR = 1.12, 95% CI: 0.97-1.30, p = 0.11) or past year MDE with severe role impairment (OR = 1.16, 95% CI: 0.98-1.37, p = 0.08). A statistically significant increase in the odds of past year MDE with alcohol use disorder (OR = 1.68, 95% CI: 0.99-2.85, p = 0.05) has been observed.
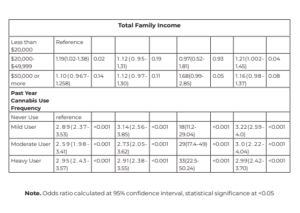
Prediction by Cannabis use Frequency
Compared to those who never used cannabis, mild, moderate, and heavy cannabis users displayed progressively higher odds of lifetime MDE, past year MDE, past-year MDE with alcohol use disorder, and past year MDE with severe role impairment.
For mild cannabis users, the odds of lifetime MDE were substantially higher (OR = 2.89, 95% CI: 2.37-3.53, p < 0.001), and this trend persisted for past year MDE (OR = 3.14, 95% CI: 2.56-3.85, p < 0.001), and past year MDE with severe role impairment (OR = 3.22, 95% CI: 2.59-4.0, p < 0.001). Similarly, moderate cannabis users exhibited increased odds for all outcomes: lifetime MDE (OR = 2.59, 95% CI: 1.98-3.41, p < 0.001), past year MDE (OR = 2.73, 95% CI: 2.05-3.62, p < 0.001), and past year MDE with severe role impairment (OR = 3.0, 95% CI: 2.22-4.04, p < 0.001).For heavy cannabis users, the odds were similarly elevated across all outcomes: lifetime MDE (OR = 2.95, 95% CI: 2.43-3.57, p < 0.001), past year MDE (OR = 2.91, 95% CI: 2.38-3.55, p < 0.001, and past year MDE with severe role impairment (OR = 2.99, 95% CI: 2.42-3.70, p < 0.001).
The study findings indicate a consistent and escalating association between past-year cannabis use frequency and the likelihood of experiencing major depressive episodes (MDE) with co-occurring alcohol use disorder among adolescents. Compared to individuals who reported never using cannabis, mild cannabis users demonstrated a substantially higher odds ratio (OR = 18.0, 95% CI: 11.2-29.04, p < 0.001) for past-year MDE with alcohol use disorder. This pattern continued for moderate cannabis users, with a dramatic increase in the odds (OR = 29.0, 95% CI: 17.4-49.0, p < 0.001). Heavy cannabis users exhibited the highest risk, with an even greater odds ratio (OR = 33.0, 95% CI: 22.5-50.24, p < 0.001).
Discussion
The Depression has been reported as a common affective adverse event in adolescent marijuana users.However, current literature remains divisive on the depression risk in adolescent marijuana users. Most literature (Bolanis et al., 2020; Chadi et al., 2019; Schoeler et al., 2018) we found showed that adolescent marijuana users had higher odds of depression even after adjusting for concomitant substance use, which contrasts with other studies (Gobbi et al., 2019) showing low risk association. Such duality of findings regarding the adolescent’s depression association with marijuana use raises the possibility that cannabis use may increase depression under certain conditions, such as other substance use, adverse childhood experience. Those conditions might not always be mutually exclusive. Our result showed greater odds of depression, depression with severe impairment, and depression with alcohol disorder in any frequency of marijuana use. This study uniquely contributes by utilizing data from a recent national survey with larger sample size and sampling weights that allow authors to approximate the young marijuana users on a national level.
This population-based study is the first, to our knowledge, to examine the if the frequency of cannabis use can predict depression, depression with severe impairment, and depression with alcohol use disorder (AUD) simultaneously during adolescence from recent NSDUH data.
On top of that, predictive probability of sociodemographic variables to depression outcome and sociodemographic and depression outcomes correlates of marijuana use have been explored (see Table 1 and 2). Our study has following main findings. Female gender and White race followed by Hispanic have statistically higher marijuana consumption while some most studies (Assari et al., 2018; Hamilton et al., 2019; Terry‐McElrath et al., 2020) reported otherwise. The gender gap was already narrowing over time (Hemsing & Greaves, 2020), and the racial sample size difference might play a role here for this finding. Significantly higher likelihood of lifetime and past year major depressive episode (MDE), MDE with severe role impairment, as well as MDE with alcohol use disorder (p < 0.01), were observed among adolescents with a history of cannabis use.
As for the subjective dimension to the cannabis consumption among adolescents, between 63% and 75% of adolescents view moderate to heavy marijuana use as not posing a significant risk, and 35% of adolescents consider acquiring marijuana to be quite accessible. As cannabis use frequency increased, predicted prevalence of lifetime and past-year MDE, past year MDE with severe role impairment, past year MDE with AUD increased significantly (p < 0.001). The moderate (12- 49 days a year) and heavy (≥50 days a year) cannabis users showed particularly elevated odds in relation to MDE with alcohol use disorder.
Overall, 13% adolescents (weighted about 3 million adolescents) reported lifetime marijuana use. Any frequency of past year marijuana use predicted both depression and depression with AUD in adolescence. As far as we are aware no studies have investigated associations from cannabis use to both severe depression and depression with alcohol use disorder simultaneously. Few studies have investigated depression to cannabis use (Hoffmann, 2018), cannabis use to depression (Hengartner et al., 2020; Lawn et al., 2022; Mustonen et al., 2021), cannabis and alcohol use to depression (Fleming et al., 2021), depression to alcohol and cannabis use disorder (Rhew et al., 2017).
Most studies in our literature search demonstrated that depression was associated with increased subsequent cannabis use, alcohol use or simultaneous use of alcohol and marijuana (SAM) during adolescence. Our study extends the current body of knowledge by predicting depression with alcohol use disorder by increasing frequency category of cannabis use (mild, moderate, heavy use) among adolescents. Compared to studies that have investigated the bidirectional associations between depression and cannabis use simultaneously, our study had the advantage of also examining alcohol use disorder and was based on a representative sample of today’s adolescents.
Our study findings bring out the hypothesis in the table of discussion that depression precedes cannabis use, whereby adolescents may use cannabis to reduce stress or relaxation (Moreno-Mansilla et al., 2021). Research also shows that the therapeutic efficacy of cannabis to alleviate negative affect is largely short-term benefit rather it increases baseline depression in long term (Cuttler et al., 2018). While adolescents might be taking marijuana, the gateway drug as a coping strategy for alleviation of stress, it increases their likelihood to consume other substance use like alcohol (Borodovsky and Budney, 2018; Scheier & Griffn, 2021).
Limitations and Strengths
Dosage of cannabis use could not be known from the NSDUH dataset; hence, the frequency of use was taken as a crude estimate. This can cause the borderline data from categories of use severity, in some instance to be intermingling given that an adolescent may consume cannabis at very high amount attributed a mild user to moderate category. The self-reported nature of data, frequency of cannabis use data may be prone to response bias and potential underreporting. The diagnosis of alcohol abuse disorder or depression were not confirmed through clinician assessment or objective measures like urine drug screen tests. Furthermore, The NSDUH data do not allow for the determination of the chronological onset sequence between Alcohol Use Disorders (SUD) and Major Depressive Episodes (MDE) among adolescents aged 12 to 17, preventing the establishment of whether SUD preceded MDE or vice versa. The authors would also like to acknowledge the presence of potential confounders especially developmental environment related factors.
Despite those limitations, the study’s strength is the large, nationally representative sample of the U.S. adolescent population aged 12 to 17. The study updates and contributes to the existing knowledge base by providing information from a recent NSDUH. The research addresses a significant gap in the literature by exploring factors associated with depression, depression with severe role impairment, or alcohol use disorder. It also investigates marijuana use frequency as a predictor for depression with Alcohol Use Disorder (AUD).
Conclusion
Our analyses identified use of marijuana as significant risk factors for all depression-related outcomes. Higher use of marijuana (moderate and heavy user) was also strongly associated with all depression outcomes, and the association with depression with alcohol use disorder was somewhat greater in magnitude than expected. Further research is needed to investigate the dose relationship between cannabis use frequency on depressive symptomatology with and without alcohol use disorder.
Misconceptions about marijuana safety and easy access might contribute to higher MDE rates among frequent users, necessitating further research on underlying motivation of substance use and youth sensitive corrective education. Clinicians should be aware that even any lifetime cannabis use in an adolescent suggests a higher likelihood of depression. Careful screening for depression and history co use of alcohol in an adolescent with any history of cannabis use should be investigated.
The limitations of NSDUH may constrain any deeper understanding between the cannabis user categories, nonetheless this work provides a starting point for further prospective research on the relationship between cannabis use frequency and affective disorders with and without polysubstance use in adolescence.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-proft sectors.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, D
Aloi, J., Meffert, H., White, S. F., Blair, K. S., Hwang, S., Tyler, P. M., Thornton, L. C., Crum, K. I., Adams, K., Killanin, A. D., Filbey, F. M., Pope, K., & Blair, R. J. R. (2019). Differential dysfunctions related to alcohol and cannabis use disorder symptoms in reward and error-processing neuro-circuitries in adolescents. Developmental Cognitive Neuroscience, 36, 100618. https://doi.org/10.1016/j. dcn.2019.100618
Assari, S., Mistry, R., Caldwell, C. H., & Zimmerman, M. A. (2018). Marijuana use and depressive symptoms; Gender differences in African American adolescents. Frontiers in Psychology, 9. https://doi. org/10.3389/fpsyg.2018.02135
Banks, D. E., Rowe, A. T., Mpofu, P., & Zapolski, T. C. B. (2017). Trends in typologies of concurrent alcohol, marijuana, and cigarette use among US adolescents: An ecological examination by sex and race/ethnicity. Drug and Alcohol Dependence, 179, 71–77. https://doi.org/10.1016/j.drugalcdep.2017.06.026
Bodden, D., Stikkelbroek, Y., & Dirksen, C. D. (2018). Societal burden of adolescent depression, an overview and cost-of-illness study. Journal of Affective Disorders, 241, 256– 262. https://doi.org/10.1016/j. jad.2018.06.015
Bolanis, D., Orri, M., Castellanos‐Ryan, N., Renaud, J., Montreuil, T., Boivin, M., Vitaro, F., Tremblay, R. E., Turecki, G., Côté, S. M., Séguin, J. R., & Geoffroy, M. (2020). Cannabis use, depression and suicidal ideation in adolescence: direction of associations in a population based cohort. Journal of Affective Disorders, 274, 1076–1083. https://doi. org/10.1016/j.jad.2020.05.136
Chadi, N., Li, G., Cerda, N., & Weitzman, E. R. (2019). Depressive symptoms and suicidality in Adolescents using e-Cigarettes and marijuana: a secondary data analysis from the Youth Risk Behavior Survey. Journal of Addiction Medicine, 13(5), 362– 365. https://doi.org/10.1097/ adm.0000000000000506
Claus, E. D., Ewing, S. W. F., Magnan, R. E., Montanaro, E., Hutchison, K. E., & Bryan, A. D. (2017). Neural mechanisms of risky decision making in adolescents reporting frequent alcohol and/or marijuana use. Brain Imaging and Behavior, 12(2), 564–576. https://doi. org/10.1007/s11682-017-9723-x
Crocker, C., Carter, A., Emsley, J. G., Magee, K., Atkinson, P., & Tibbo, P. G. (2021). When cannabis use goes wrong: Mental health side effects of cannabis use that present to emergency services. Frontiers in Psychiatry, 12. https://doi.org/10.3389/ fpsyt.2021.640222
Cuttler, C., Spradlin, A., & McLaughlin, R. J. (2018). A naturalistic examination of the perceived effects of cannabis on negative affect. Journal of Affective Disorders, 235, 198– 205. https://doi.org/10.1016/j. jad.2018.04.054
Fleming, C. B., Duckworth, J. C., Rhew, I. C., Abdallah, D. A., Guttmannova, K., Patrick, M. E., & Lee, C. M. (2021). Young adult simultaneous alcohol and marijuana use: Between- and within-person associations with negative alcohol-related consequences, mental health, and general health across two-years. Addictive Behaviors, 123, 107079. https://doi.org/10.1016/j.addbeh.2021.107079
Gajos, J. M., Purcell, J. B., & Mrug, S. (2021). The Intersection between Sex and Race in understanding Substance Co-USe Patterns in Adolescents from the Fragile Families study. Journal of Drug Issues, 52(1), 15–30. https://doi. org/10.1177/00220426211041093
Gobbi, G., Atkin, T., Zytynski, T., Wang, S., Askari, S., Boruff, J., Ware, M. A., Marmorstein, N. R., Cipriani, A., Dendukuri, N., & Mayo, N. E. (2019). Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood. JAMA Psychiatry, 76(4), 426. https:// doi.org/10.1001/jamapsychiatry.2018.4500
Gukasyan, N., & Strain, E. C. (2020). Relationship between cannabis use frequency and major depressive disorder in adolescents: Findings from the National Survey on Drug Use and Health 2012–2017. Drug and Alcohol Dependence, 208, 107867. https://doi.org/10.1016/j. drugalcdep.2020.107867
Hamilton, A., Jang, J. B., Patrick, M. E., Schulenberg, J. E., & Keyes, K. M. (2019). Age, period and cohort effects in frequent cannabis use among US students: 1991–2018. Addiction, 114(10), 1763–1772. https://doi. org/10.1111/add.14665
Hammond, C., Chaney, A., Hendrickson, B. P., & Sharma, P. (2020). Cannabis use among U.S. adolescents in the era of marijuana legalization: a review of changing use patterns, comorbidity, and health correlates. International Review of Psychiatry, 32(3), 221–234. https://doi.org/10.1080/0954026 1.2020.1713056
Hemsing, N., & Greaves, L. (2020). Gender Norms, Roles and Relations and Cannabis-Use Patterns: A Scoping review. International Journal of Environmental Research and Public Health, 17(3), 947. https:// doi.org/10.3390/ijerph17030947
Hengartner, M. P., Angst, J., Ajdacic-Gross, V., & Rössler, W. (2020). Cannabis use during adolescence and the occurrence of depression, suicidality and anxiety disorder across adulthood: Findings from a longitudinal cohort study over 30 years. Journal of Affective Disorders, 272, 98–103. https:// doi.org/10.1016/j.jad.2020.03.126
Hines, L. A., Freeman, T. P., Gage, S. H., Zammit, S., Hickman, M., Cannon, M., Munafò, M. R., Macleod, J., & Heron, J. (2020). Association of High Potency cannabis use with mental health and substance use in adolescence. JAMA Psychiatry, 77(10), 1044. https:// doi.org/10.1001/jamapsychiatry.2020.1035
Hoffmann, J. P. (2018). Marijuana Use and Depressive Symptoms among Young People: Examining Unidirectional and Bidirectional Effects. Health, 10(08), 1066– 1078. https://doi.org/10.4236/ health.2018.108080
Jones, C. M., & McCance‐Katz, E. F. (2019). Relationship between recency and frequency of youth cannabis use on other substance use. Journal of Adolescent Health, 64(3), 411–413. https://doi.org/10.1016/j. jadohealth.2018.09.017
Lawn, W., Mokrysz, C., Lees, R., Trinci, K., Petrilli, K., Skumlien, M., Borissova, A., Ofori, S., Bird, C., Jones, G., Bloomfeld, M., Das, R., Wall, M. B., Freeman, T. P., & Curran, H. V. (2022). The CannTeen Study: Cannabis use disorder, depression, anxiety, and psychotic-like symptoms in adolescent and adult cannabis users and age-matched controls. Journal of Psychopharmacology, 36(12), 1350–1361. https://doi. org/10.1177/02698811221108956
Langlois, C. C., Potvin, S., Khullar, A., & Tourjman, S. V. (2021). Down and high: Refections regarding depression and cannabis. Frontiers in Psychiatry, 12. https://doi.org/10.3389/ fpsyt.2021.625158
Leon, A. C., Olfson, M., Portera, L., Farber, L. H., & Sheehan, D. V. (1997). Assessing Psychiatric Impairment in Primary Care with the Sheehan Disability Scale. The International Journal of Psychiatry in Medicine, 27(2), 93–105. https://doi.org/10.2190/ t8em-c8yh-373n-1uwd
Lipperman‐Kreda, S., Gruenewald, P. J., Grube, J. W., & Bersamin, M. (2017). Adolescents, alcohol, and marijuana: Context characteristics and problems associated with simultaneous use. Drug and Alcohol Dependence, 179, 55–60. https://doi.org/10.1016/j.drugalcdep.2017.06.023
McHugh, R. K. (2019). Alcohol use disorder and depressive disorders. Alcohol Research, 40(1). https://doi.org/10.35946/ arcr.v40.1.01
Mojtabai, R., Olfson, M., & Han, B. (2016). National Trends in the Prevalence and Treatment of Depression in Adolescents and Young Adults. Pediatrics, 138(6). https://doi.org/10.1542/ peds.2016-1878
Moreno-Mansilla, S., Ricarte, J. J., & Hallford, D. J. (2021). Cannabis use among early adolescents and transdiagnostic mental health risk factors. Clinical Child Psychology and Psychiatry, 26(2), 531–543. https://doi. org/10.1177/1359104521994637
Mustonen, A., Hielscher, E., Miettunen, J., Denissoff, A., Alakokkare, A., Scott, J. G., & Niemelä, S. (2021). Adolescent cannabis use, depression and anxiety disorders in the Northern Finland Birth Cohort 1986. British Journal of Psychiatry Open, 7(4). https://doi. org/10.1192/bjo.2021.967
Nugent, S. M., Yarborough, B. J. H., Smith, N., Dobscha, S. K., Deyo, R. A., Green, C. A., & Morasco, B. J. (2018). Patterns and correlates of medical cannabis use for pain among patients prescribed long-term opioid therapy. General Hospital Psychiatry, 50, 104–110. https://doi.org/10.1016/j.genhosppsych.2017.11.001
Pasman, J. A., Verweij, K. J. H., Gerring, Z., Stringer, S., Sanchez‐Roige, S., Treur, J. L., Abdellaoui, A., Nivard, M. G., Baselmans, B. M. L., Ong, J., Ip, H. F., Van Der Zee, M. D., Bartels, M., Day, F. R., Fontanillas, P., Elson, S. L., De Wit, H., Davis, L. K., MacKillop, J., . . . Vink, J. M. (2018). GWAS of lifetime cannabis use reveals new risk loci, genetic overlap with psychiatric traits, and a causal effect of schizophrenia liability. Nature Neuroscience, 21(9), 1161–1170. https://doi.org/10.1038/s41593- 018-0206-1
Patalay, P., & Gage, S. H. (2019). Changes in millennial adolescent mental health and health-related behaviours over 10 years: a population cohort comparison study.International Journal of Epidemiology, 48(5), 1650–1664. https://doi. org/10.1093/ije/dyz006
Pedroni, C., Dujeu, M., Lebacq, T., Desnouck, V., Holmberg, E., & Castetbon, K. (2021). Alcohol consumption in early adolescence: Associations with sociodemographic and psychosocial factors according to gender. PLOS ONE, 16(1), e0245597. https://doi.org/10.1371/journal. pone.0245597
Ramlagan, S., Peltzer, K., & Pengpid, S. (2021). Prevalence and correlates of non-daily and daily cannabis use among persons 15 years and older in South Africa: results of a national survey in 2017. Substance Abuse Treatment, Prevention, and Policy, 16(1). https://doi. org/10.1186/s13011-021-00364-z
Reece, A. S., & Hulse, G. K. (2020). Co-occurrence across time and space of drug- and cannabinoid- exposure and adverse mental health outcomes in the National Survey of Drug Use and Health: combined geotemporospatial and causal inference analysis. BMC Public Health, 20(1). https://doi. org/10.1186/s12889-020-09748-5
Rhew, I. C., Fleming, C. B., Stoep, A. V., Nicodimos, S., Zheng, C., & McCauley, E. (2017). Examination of cumulative effects of early adolescent depression on cannabis and alcohol use disorder in late adolescence in a community‐based cohort. Addiction, 112(11), 1952–1960. https://doi.org/10.1111/add.13907
Scheier, L. M., & Griffn, K. W. (2021). Youth marijuana use: a review of causes and consequences. Current Opinion in Psychology, 38, 11–18. https://doi.org/10.1016/j.copsyc.2020.06.007
Schoeler, T., Theobald, D., Pingault, J., Farrington, D. P., Coid, J. W., & Bhattacharyya, S. (018). Developmental sensitivity to cannabis use patterns and risk for major depressive disorder in mid-life: fndings from 40 years of follow-up. Psychological Medicine, 48(13), 2169–2176. https://doi. org/10.1017/s0033291717003658
Siddiqui, S. A., Singh, P., Khan, S., Fernando, I., Baklanov, I. S., Ambartsumov, T. G., & Ibrahim, S. A. (2022). Cultural, Social and Psychological Factors of the Conservative Consumer towards Legal Cannabis Use—A Review since 2013. Sustainability, 14(17), 10993. https://doi.org/10.3390/ su141710993\
Ssegonja, R., Alaie, I., Philipson, A., Hagberg, L., Sampaio, F., Möller, M., Von Knorring, L., Sarkadi, A., Langenskiöld, S., Von Knorring, A., Bohman, H., Jönsson, U., & Feldman, I. (2019). Depressive disorders in adolescence, recurrence in early adulthood, and healthcare usage in mid-adulthood: A longitudinal cost-of-illness study. Journal of Affective Disorders, 258, 33–41. https://doi. org/10.1016/j.jad.2019.07.077
Substance Abuse and Mental Health Services Administration. (2022). Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/ data/report/2021-nsduh-annual-national-report
Terry‐McElrath, Y. M., O’Malley, P. M., & Johnston, L. D. (2020). The growing transition from lifetime marijuana use to frequent use among 12th grade students: U.S. National data from 1976 to 2019. Drug and Alcohol Dependence, 212, 108064. https://doi.org/10.1016/j. drugalcdep.2020.108064
Thompson, K., Holley, M., Sturgess, C., & Leadbeater, B. J. (2021). Co-Use of Alcohol and Cannabis: Longitudinal Associations with Mental Health Outcomes in Young Adulthood. International Journal of Environmental Research and Public Health, 18(7), 3652. https://doi. org/10.3390/ijerph18073652
Twenge, J. M. (2020). Why increases in adolescent depression may be linked to the technological environment. Current Opinion in Psychology, 32, 89–94. https://doi.org/10.1016/j. copsyc.2019.06.036
Weinberger, A. H., Zhu, J., Lee, J., Anastasiou, E., Copeland, J., & Goodwin, R. D. (2020). Cannabis use among youth in the United States, 2004–2016: Faster rate of increase among youth with depression. Drug and Alcohol Dependence, 209, 107894. https://doi.org/10.1016/j.drugalcdep.2020.107894
White, H. R., Kilmer, J. R., Fossos-Wong, N., Hayes, K. L., Sokolovsky, A. W., & Jackson, K. M. (2019). Simultaneous alcohol and marijuana use among college students: patterns, correlates, norms, and consequences. Alcohol: Clinical & Experimental Research, 43(7), 1545–1555. https:// doi.org/10.1111/acer.14072
Zuckermann, A. M., Battista, K., De Groh, M., Jiang, Y., & Leatherdale, S. T. (2019). Pre-legalization patterns and trends of cannabis use among Canadian youth: results from the COMPASS prospective cohort study. BMJ Open, 9(3), e026515. https://doi.org/10.1136/ bmjopen-2018




