Research Objectives:
EIdeas on how to harness digital health technology in the fight against cancer and thus benefit from others digital health innovations are the core aims of this research paper.
Keywords:
Cancer, Health, Digital, Technology
Bio
Roxanne Boodhoo is an accomplished professional with a diverse and versatile background. Her extensive academic training has equipped her with a wide range of skills and knowledge, enabling her to excel in various roles. Roxanne is known for her strong work ethic, diligence, and commitment to undertaking any responsibilities assigned to her. She is deeply passionate about helping and supporting others, making her a compassionate and empathetic individual. Throughout her career, Roxanne has consistently demonstrated a dedication to making a positive impact, whether through her professional work or community involvement, striving to uplift those around her.
Abstract
Recent years have witnessed significant advancements in radiation therapy, driven by developments in photon, electron, and proton radiations, as well as the emerging use of hypo fractionated applications. Despite these innovations, the future of fractionated radiation oncology remains secure due to the complexities involved in maximising therapeutic gains without increasing toxicity. Concurrently, infammatory bowel diseases, particularly ulcerative colitis, play a crucial role in both gross and microscopic findings in differential diagnoses. Initial diagnostic approaches often involve evaluating antibiotic-resistant or induced enteritis through therapy history and PCR testing for Clostridium diffcile. Persistent clinical symptoms suggestive of therapy resistance or re-infection necessitate further testing for Clostridium diffcile fecal toxins.
Cancer therapy is increasingly influenced by digital advancements and innovative biomedical technologies. Significant progress has introduced novel diagnostic and therapeutic tools, including laser technology for surgery, photodynamic therapy, and bio-imaging. Additionally, nanotechnology has revolutionised potential therapies, enabling selective multimodal tumor diagnostics and treatment. This approach combines contrast enhanced imaging with targeted therapy, opening new horizons in cancer treatment.
The scientific community is actively developing and establishing advanced nanotechnology-based nanomedicines, reflecting a concerted effort to enhance cancer therapy. The integration of these cutting-edge technologies promises to improve diagnostic accuracy and therapeutic outcomes, driving the future of cancer treatment towards more precise and effective interventions.
Introduction
The clinical application of AI in oncologic radiation therapy demonstrated its capacity to improve the diagnosis, treatment, and prognosis of cancer (Casà et al., 2023). Three main features AI manifested, including the NPaware, Hardware-aware, and high-throughput data processing. The AI/ML models presented the potential as robust biomarkers in reducing heterogeneity in treatment response and improve the general effectiveness of immunotherapy.
A cohort of promising AI/ML models were developed to diagnose tumours, determine the DNA damage response, identify synthetic lethal interactions, and predict immunotherapy response. In radiotherapy machine learning was successfully implemented for detecting novel radiomic features, automatically contouring organs, the classification of target volume delineation and organs at risk delineation and models for neoadjuvant chemotherapy in head and neck cancer. Novel caDISC members were identified that showed prognostic value in endometrial cancer.
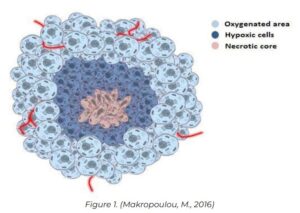
Figure 1 illustrated a Schematic representation of a multi-cellular solid tumor. The tumor exhibits a quasi-spherical shape with a concentric arrangement of cells. Aerobic and proliferating tumor cells are situated on the periphery, while a smaller fraction of non-proliferating cells are found in deeper regions, encircling a core of dead cells (central necrotic core). This necrotic core results from cell death caused by restricted oxygen and nutrient diffusion.
Use of AI in designing individualised therapeutic options for leukaemia and other types of cancer, which has evolved rapidly over the years, including RPs, signal transduction, functional genomics, and immunogenomics, among others. Among different types of cancer, leukaemia is one of the exploitations of digital tools, varying from case finding, diagnosis, treatment, follow-up and survivorship, to end of life care. it is anticipated in the United States that by 2030, there will be a 269% increase in the number of adult survivors of childhood cancer with a similar absolute increase in the number of survivors with a history of haematological malignancies. As a result, two new brief surveys have been developed for this valuable cohort to assess their cancer and treatment-related problems.
Aim
Ideas on how to harness digital health technology in the fight against cancer and thus benefit from others digital health innovations are the core aims of this paper. Some perspectives on this are given per se, others are inspired by digital health inventions that deal with other diseases. This paper hopes to describe areas for future digital health research and development in under-served countries and other low-resource spheres with a strong focus on cost-effective measures.
One in six deaths worldwide is due to one of the 200 types of cancer (Patel et al., 2023) (Makropoulou, 2016). In 2040, the predicted global cancer burden may almost double, reaching 30 million new cases per year (World Health Organization, 2020). High-income countries averagely invest 1.9% among their gross domestic product (GDP) into their cancer care systems greatly supported by digital health technology (Darley et al., 2023). Such funding, however, is unrealistic in low-income countries, which not only have to deal with unproportionally high cancer incidence rates, but also need to educate most people on how to prevent cancer and thus avoid particularly high costs for direct cancer care. Considering cost-effective health care, educational measures informed by digital health technology could achieve a lot in low-income countries as well. At the same time, the developing countries could serve as a sandbox environment for new digital health approaches, before being used in a proper health environment in high-income countries.
Method
It is critical to generate and continuously improve evidence to support the use of telemedicine and electronic communications in good clinical practice. Additionally, the evaluation of the usability and acceptability of interventions that can be part of digitization as a change process in healthcare must be considered. The cancer care pathway must be seamless, avoiding fragmentation due to digitization. After input from healthcare professionals, the patient and user perspective must take a central position in conjunction with the edu cation and insight of healthcare staff. It will be important to include the users (and also the patient) in the assessment of digital tools’ practical suitability. The digital tools should be cost effective for both peoples’ health and the health economy, with focus on the utilities. Great improvement in cancer patients’ reported outcomes of treatment and treatment choices will be a key measure (Andrades & Recamonde-Mendoza, 2021).
The guiding principles for the introduction of innovation, evaluation and implementation of new technologies, and good digital technology practice in the National Health Service (NHS) should be based on care pathways and needs, cost effectiveness and equality (C. Griffn et al., 2020). Patient reported outcome measures (PROMs), including health-related quality of life, functional capacity, pain assessment and symptom-related follow-up, should be utilised to establish the quality of patient care on digital platforms. These measures should apply to any intervention or drug, an occurrence in all diseases and changes in statistics on common diseases, for example cancer, should be observed. Patients should be involved in setting the parameters for utility.
Results and Discussion
At the time of writing, m-health is playing a vital role in contributing to healthcare by offering a convenient and efficient way to replace or complement traditional in-person interactions. This is especially beneficial in the field of oncology care, where physical interactions are crucial for the accurate delivery of complex testing and treatment plans. As it has already been successfully demonstrated, digital solutions, particularly the use of smartphones and mobile applications, have the ability to avoid unnecessary hospital visits, greatly improve patients’ overall experiences, enhance adherence to follow-up treatment, and facilitate significant time savings for both patients and healthcare providers alike. The utilisation of advanced algorithms and smart programming further allows for the seamless adjustment of the next steps in the pathway of care for patients, all based on their ongoing monitoring data and through online consultations. Additionally, it is worth noting that the majority of diagnostic image facilities worldwide still rely on non-digital methods, which unfortunately limits access to remote experts and timely distant review (Agarwal et al., 2020). This further emphasises the urgent need for embracing digital technology in healthcare to ensure optimal patient outcomes are consistently achieved.
While any amount of liver cancer is something to be concerned about, in emerging economies, the majority of patients present with more advanced stages at the time of diagnosis. However, smartphones are ubiquitous in most emerging countries and could be efficiently utilised in a solution to address obstacles in the continuum of care for liver cancer patients (Huang et al.2022). With specifically trained and deployed digital health workers from within, in parallel with leveraging widely available local care resources, we can develop and implement a novel digital health strategy that aims to support health and education system strengthening. By utilising the vast potential of mobile technology, we can revolutionise the way liver cancer patients receive care and support in emerging economies. With smartphones being pervasive in these countries, there is an unprecedented opportunity to bridge the gap between patients and healthcare providers. Combining the power of digital health workers who have been trained for this specific purpose and making use of existing local healthcare resources, we can create a groundbreaking digital health strategy that not only provides assistance but also strengthens the overall health and education system. Through the integration of smartphones into the continuum of care, we can ensure that liver cancer patients have access to vital information, resources, and support at all stages of their journey. By deploying a network of highly skilled digital health workers, who are equipped with the knowledge to navigate through the complexities of liver cancer care, we can overcome the barriers that hinder timely diagnosis and treatment (Wazir et al.2023). Moreover, by tapping into the readily available local care resources, we can create a synergy that boosts the overall healthcare infrastructure in emerging economies, leading to improved outcomes for liver cancer patients.
This innovative digital health strategy holds immense potential to transform the landscape of liver cancer care in emerging economies. By harnessing the power of smartphone technology and utilising the expertise of digital health workers, we can pave the way for a more inclusive and comprehensive approach to tackling this devastating disease. Through the seamless integration of mobile devices, local resources, and a well-trained workforce, we can achieve unparalleled advancements in health and education system strengthening, ultimately benefiting not only liver cancer patients but the entire population as well. With the implementation of this game-changing digital health strategy, individuals facing liv er cancer in emerging economies will experience a significant improvement in their overall care and outcomes. The utilisation of smartphones, which have become an integral part of everyday life in these countries, allows for a unique opportunity to bridge the divide between patients and healthcare providers (Potdar et al.2020). By capitalising on the expertise and training of digital health workers who are dedicated to liver cancer care, alongside the utilisation of existing local healthcare resources, a ground-breaking and effective digital health strategy can be established.
By incorporating smartphones into the continuum of care, liver cancer patients will have continuous access to the vital information, resources, and support that they require at every step of their journey. Through the formation of a network of highly skilled digital health workers, equipped with the necessary knowledge and expertise to navigate the intricacies of liver cancer care, the barriers to early diagnosis and treatment can be effectively overcome. Additionally, by optimising the readily accessible local care resources, a symbiotic relationship can be established, further bolstering the overall healthcare infrastructure in emerging economies, ultimately benefiting liver cancer patients and the wider population.
The implementation of this innovative digital health strategy has the potential to completely revolutionise the landscape of liver cancer care in emerging economies. By harnessing the power of smartphone technology and leveraging the specialised skills of digital health workers, a truly inclusive and comprehensive approach to combating this debilitating disease can be crafted (Lv et al., 2023). Through the seamless integration of mobile devices, local resources, and a highly skilled workforce, unprecedented advancements in health and education system strengthening can be achieved. This, in turn, will not only significantly benefit liver cancer patients but will also have a profound and lasting impact on the overall wellbeing of the entire population.
Conclusion
This study has critically explored how existing digital technologies are effectively configured to be optimised for enhanced prevention; prehabilitation (of the human subject), detection (including early diagnosis), treatment, and care, in the fight against cancer. More specifically, it has been established that the declarative use of digital technologies for the fight against cancer, from an ethical and regulatory perspective. As new warfronts emerge in the fight against the development and progression of cancer, a critical at the leverage of digital technologies and systems in effectively fighting these warfronts becomes inevitable. Indeed, this article sets out with the explicit aim of critically evaluating the use and effective employment of these set of digital technologies in the fight against cancer, including some of the futuristic endeavours being charted within research environments through social inclusion. (Patel et al., 2023)
Increased cancer incidence, prevalence, costs, and deaths threaten the quality of life globally (Makropoulou, 2016). As the cancer burden has proven to be multidimensional, a multi-pronged strategy to combat this scourge that includes cancer prevention, detection, treatment, and care must be adopted. Emerging advancements in digital technologies such as the Internet of Things (IoTs), Artificial Intelligence (AI) for hepatocellular carcinoma (AIHCC), Machine learning (ML), and Big Data presages the potential future of electronic healthcare that leverages data-driven solutions.
References
Agarwal, S., Singh Punn, N., Kumar Sonbhadra, S., Tanveer, M., Nagabhushan, P., K Soundra Pandian, K., & Saxena, P. (2020). Unleashing the power of disruptive and emerging technologies amid COVID-19: A detailed review. [PDF]
Andrades, R. & Recamonde-Mendoza, M. (2021). Machine learning methods for prediction of cancer driver genes: a survey paper. [PDF]
Griffn, A., Topaloglu, U., Davis, S., & E. Chung, A. (2020). From Patient Engagement to Precision Oncology: Leveraging Informatics to Advance Cancer Care. ncbi.nlm.nih.gov
Casà, C., Dinapoli, L., Marconi, E., Chiesa, S., Cornacchione, P., Beghella Bartoli, F., Bracci, S., Salvati, A., Scalise, S., Ferdinando Colloca, G., Pia Rosaria Chieffo, D., Antonietta Gambacorta, M., Valentini, V., & Tagliaferri, L. (2023). Integration of art and technology in person alized radiation oncology care: Experiences, evidence, and perspectives. ncbi.nlm.nih.gov
Charalambous, A. (2019). Utilizing the Advances in Digital Health Solutions to Manage Care in Cancer Patients. ncbi.nlm.nih.gov
Darley, A., Coughlan, B., Maguire, R., McCann, L., & Furlong, E. (2023). A bridge from uncertainty to understanding: The meaning of symptom management digital health technology during cancer treatment.ncbi.nlm.nih.gov
Huang, D. Q., Singal, A. G., Kono, Y., Tan, D. J., El-Serag, H. B., & Loomba, R. (2022). Changing global epidemiology of liver cancer from 2010 to 2019: NASH is the fastest growing cause of liver cancer. cell.com
Lv, L., Zhao, B., Kang, J., Li, S., & Wu, H. (2023). Trend of disease burden and risk factors of breast cancer in developing countries and territories, from 1990 to 2019: Results from the Global Burden of Disease Study …. Frontiers in Public Health. . frontiersin.org
Makropoulou, M. (2016). Cancer and electromagnetic radiation therapy: Quo Vadis?. [PDF]
Patel, S., C Goldsack, J., Cordovano, G., Downing, A., K Fields, K., Geoghegan, C., Grewal, U., Nieva, J., Patel, N., E Rollison, D., Sah, A., Said, M., Van De Keere, I., Way, A., L WolffHughes, D., A Wood, W., & J Robinson, E. (2023). Access to internet, smartphone usage, and acceptability of mobile health technology among cancer patients. Supportive Care in Cancer, 28, 5455-5461. medrxiv.org
Rasheed, S., Kanwal, T., Ahmad, N., Fatima, B., Najamul-Haq, M., & Hussain, D. (2024). Advances and challenges in portable optical biosensors for onsite detection and point-of-care diagnostics. TrAC Trends in Analytical Chemistry, 117640. [HTML]
Wazir, H., Abid, M., Essani, B., Saeed, H., Khan, M. A., Nasrullah, F. N. U., … & ahad Shah, A. (2023). Diagnosis and Treatment of Liver Disease: Current Trends and Future Directions. Cureus, 15(12). cureus.com