Research Objectives:
This study aims to explore the potential of combining Manual Lymphatic Drainage (MLD) and grounding therapies to enhance cognitive function, reduce neuroinflammation, and improve brain resilience in Alzheimer’s disease through improved lymphatic and neuroimmune interactions.
Keywords:
Manual Lymphatic Drainage (MLD), Alzheimer’s Disease (AD), neuroinflammation, grounding therapy, cognitive health.
Bio
Phyllis A. Nunn is a renowned author, speaker, trauma trainer, and Harvard Fellow. As a sought-after Neuromuscular Massage insurance provider for the VA Community Care Network, she specialises in behavioural and physical rehabilitation therapies that soothe the central nervous system and reduce inflammation. Her expertise in calming therapeutic techniques has made her a respected figure in her field. Phyllis is also a proud mother, supporting her son Joshua as he pursues his doctoral degree at Rensselaer Polytechnic Institute in Troy, NY. Her dedication to healing and education reflects her deep commitment to improving the lives of others.
Abstract:
Recent advancements in Manual Lymphatic Drainage (MLD), combined with grounding therapies, offer new avenues for enhancing brain health and resilience, particularly in age-related neurodegenerative diseases such as Alzheimer’s disease (AD). In 2024, researchers uncovered a network of lymphatic vessels behind the nose responsible for draining cerebrospinal fluid (CSF), which holds significant implications for improving toxin clearance and reducing neuroinflammation in AD. The recognition of Alzheimer’s as an autoimmune condition (AD2) shifts the perspective on amyloid-beta (Aβ), traditionally considered a toxic protein, to its role as an immunomodulatory cytokine. In this model, Aβ’s antimicrobial function triggers a misdirected attack on neurons, leading to a chronic, self-perpetuating cycle of inflammation and neural damage.
MLD therapy, particularly craniofacial techniques, has been shown to enhance lymphatic drainage, reduce amyloid-β deposition, and improve mitochondrial metabolic homeostasis. These effects help to preserve the integrity of lymphatic vessels, ultimately promoting cognitive function and reducing brain swelling. The combination of lymphatic drainage and grounding methods has demonstrated promise in maintaining cognitive health, particularly in mouse models of Alzheimer’s disease. These findings suggest MLD could become a cornerstone of non-pharmacological treatment strategies aimed at enhancing brain resilience, reducing neuroinflammation, and improving overall quality of life for individuals with Alzheimer’s and related disorders, only if the masses are encouraged to add these techniques to daily exercise regimens when endorsed by mainstream media.
-
Introduction
Alzheimer’s disease is the most common cause of dementia in older adults. It affects regions of the brain involved in thinking, memory, and language. Although much is known about Alzheimer’s disease, the cause is unclear. One risk factor for the onset of Alzheimer’s disease is older age. Symptoms of Alzheimer’s disease, including memory loss and problems with other intellectual abilities such as reasoning, language, and visual perception, may become severe enough to interfere with daily life (Scheltens et al.2021). Unfortunately, currently available pharmaceuticals often either are of limited benefit or are only able to slow the progression of Alzheimer’s disease, lacking the ability to increase the quality of life for those with the disorder. By enhancing the functioning of the glymphatic system, this treatment may provide individuals with Alzheimer’s disease relief from symptoms including non-verbal confusion, increasing the likelihood that families can care for loved ones in the ease of their own home environment rather than in institutionalised settings.
1.1. Background of Alzheimer’s Disease (AD) and Current Treatment Challenges
Alzheimer’s disease (AD) is a progressive and fatal neurodegenerative disease that strikes half of those aged over 85 years. In 2016, the number of individuals living with AD dementia was estimated to be 5.4 million in the U.S., with a projected estimate of 13.9 million in 2060. These estimates may underestimate the true prevalence and burden of the disease, the cost of which exceeds 236 billion (Crestini et al.2022). There is currently no treatment to slow or arrest the course of the disease. The reasons for the lack of effective treatments are numerous, but as AD is a complex disease involving interactions between genetic and non-genetic risk factors, our incomplete understanding of AD pathogenesis underlies this shortcoming as well. Efforts to more fully understand the complex etiology of AD continue.
A promising new understanding of AD involves the neuroimmunology of the disorder. Disruption of normal neuroimmune function is an early pathological event that has been identified as a probable cause of AD and one that is common in many forms of neurodegeneration. Useful insight has recently come from studies of the lymphatic system of the brain. It was long believed that, unlike other organs, the brain lacks a lymphatic system, which is important for removing metabolic waste products, such as amyloid-β, the ingredient of the plaques that typify AD, from the brain (Jorfi et al., 2023). Instead, it was proposed that the glymphatic system cleans the brain. The glymphatic system consists of glial cells in brain microvessels that provide a pathway for the removal of waste substances from the brain through the exchange of cerebrospinal fluid and extracellular interstitial fluid. Ample evidence now exists that both these systems operate in the brain. Research into the brain lymphatic system, its role in health and disease, and the dysfunctional neuroimmune interactions it gives rise to are currently the focus of new therapeutic strategies for AD.
1.2. Emergence of Lymphatic Drainage Therapy as a Potential Intervention
Dysfunction of perineural lymphatic drainage of the brain has been proposed as an early pathogenic event in Alzheimer’s disease and all its potential subtypes. This research explores why the existing approaches to diagnosis and prevention of this purported initial failure are poorly informed and rely instead on late secondary endpoints, and how existing lymphatic-based therapeutic approaches to Alzheimer’s disease are primarily represented by a relatively small number of pathogen-informed disruptive end-stage vascular interventions of immunomodulation and drainage alone, most of which are poorly regulated, invasive, and have poorly defined interactions (Xu et al.2023). This shortcoming of current health practices also lies in stark contrast to the rapid increase in our knowledge of neuroimmune interactions brought about by ongoing discoveries of the importance and diversity of central nervous system immune modulation. These are dominated by a need for a more detailed understanding of central nervous system-specific needs and functioning of lymphatic drainage and protection, contrasting with the many non-central nervous system-specific postmortem biased studies and peripheral-derived methods by which current knowledge has been largely generated. The recent successes and potential of alternative yet equally effective nonpharmaceutical-based physiological brain targeting health therapies, to answer this and other fundamental immune and cerebrovascular brain questions—terms advanced here as ‘protocol pathways.’
Aim of the Study
An expansion of knowledge in seeking to treat, delay, or prevent the progression of Alzheimer’s disease amidst a growing Alzheimer’s population. This study will aid initiatives at an onus level to focus on the prevention of the progression of the disease among patients and carriers of this genetic abnormality. Assisting in developing parameters for preventative treatment options in this area of research will propel the foundation toward its goal of preserving a cognitively normal lifestyle for carriers of this genetic abnormality. The outreach and study of this intervention may also have benefits and preventative stimulation in the population as a whole. This research study is important for prevention techniques in genetic carrying populations with high genetic potential for early onset Alzheimer’s disease and for the prevention of the general population with a targeted analysis therapy by lessening microglial activation with grounding and other lymphatic releasing therapies. Treatment is the operative word to slow progression or to completely intervene in the disease course.
-
Methodology
We propose that stimulating the autonomic nervous system with a modulation of the immune system can avert or ameliorate memory impairment and other Alzheimer’s disease symptoms. Both the hypothesis of through-body connective signal propagation and the proposal of grounding the nervous system make specific and testable predictions. Longitudinal intervention studies, experimental designs, and mechanistic studies are proposed. Longitudinal intervention studies with aging populations aim to measure the effect of increases in plasma and tissue copper on cardiovascular health and age-related memory decline, and to investigate physical grounding and grounding supplements as participants use them in their daily lives. These studies can incorporate AD biomarkers and serum inflammatory cytokine analyses, as well as assessments of memory function and the use of an indirect measure like section thickness on retinal scans as a potential predictor of good outcomes. Experimental designs aim to measure the effect of antioxidant supplements, physical grounding, or both on cognition, as well as on the expression of inflammatory cytokines in rodent models of AD. These designs would replicate addressing humans at risk for or diagnosed with AD and produce an overall behavioural classification designed to reveal connections between cognition and brain copper dismutation. The third kind of study proposed for different but overlapping populations is mechanistic. We seek to determine how grounding mediates changes in our variously different aging bodies. This study has both animal and human aspects. The text expands upon the abstract by presenting the state of the art in grounding knowledge and explaining how the physical connection between humans and the Earth enables modulation of the immune systems of both. Addressing characteristics of immune-inflammatory activation in AD, studies are proposed to measure the response to such immune modulation, both in labelled cells and in AD rodent models, and in AD clinical cohorts, making memory function a comparison parameter.
2.1. Literature Review on Lymphatic Drainage Therapy and Grounding Approaches in AD
There has only been minimal attention given to new advancements within the area of osteopathic work, with special focus on the use of osteopathic therapies such as lymphatic drainage and grounding work that complements the osteopathic work by providing stimulating stimuli to the synergistic connections within the nervous system. The department has also encouraged clients involved in the clinical work to seek relaxation and cognitive enrichment in the comfort of eastern origins, including tai chi, yogic breathing exercises, and other cognitively stimulating exercise and nutrition practices that complement the physical work that is accomplished. Some simple, very successful grounding techniques often employed include incorporating grounding stones in sessions where clients are experiencing cognitive disturbances, being located in spaces that emanate calming natural colors, and actual massage focus within the craniosacral fluid dynamic (Esteves et al., 2022). Multiple changes, both with quantitative results and qualitative results, were the impetus behind the development of a trial that would incorporate both the positive central nervous system biomechanical alteration of cranial osteopathic adjustments with actual mechanistic lymphatic drainage. This trial should also display results that would enhance both the time of positive apprehension and the level of neurogenesis within the hippocampal region of Alzheimer’s clients.
2.2. Research Design
Pre-intervention screening with a demographic survey, the Mini-Mental State Examination, a standardised depressive measure, and the Hamilton Depression Scale will include a symptom survey, the Alzheimer’s Disease Cooperative Study – Activities of Daily Living Inventory, and a Glogau-Ivey Questionnaire. The maximum 33% of exceptions of each rating scale gold standard shall be permitted in this study. AD/A-TBI and NCI pre-intervention shall undergo neurological exclusion criteria to assess the involvement of the subjects in the trials. Washout requirements are in accordance with neurological exclusion criteria and will be chosen based on the categories of inclusion. Participants could take part in the trials anytime from two months to a year. (Khan et al.2023)
Six wards will administer the 30-minute lymphatic breast treatment in the adult day centre. The light touching approach, two-handed gliding will carry out the lymphatic breast therapy, starting from both places to sit by softly pressing the hands by the nose. The hands at the armpits will progress. Then the shoulders shall be moved by relaxing the fingertips down from the shoulders to the clavicle. The posture lung, the eccentric circular scapula origin, will be gently stroked with the fingertips. If the subject is relaxed, the assessor will indicate, and the next treatment site will continue (Lepomäki, 2023). The treatment will develop to the base of the skull and be distributed throughout the treatment. All subject assessments throughout the sessions may be performed by the assessor. Any observer will record the number of presumed discomfort responses during and following the treatment at the same time. A qualitative evaluation of the act, as well as any adverse reactions, will also be noted.
-
Results and Discussion
This research paper discusses additional treatments for Alzheimer’s disease. The suggested approach is to combine strategies of grounding using derived physiotherapeutic tools for chronic disease treatment, which promotes the need for new neural rehabilitation protocols and does not have side effects on already prescribed therapies for specific pathologies. Currently, such diseases do not have classical solutions for their healing, and human bodies have the biological adaptive capacity to be self-healed due to brain plasticity (Kölliker et al.2022). The cytoskeletal protein neurofilament light chain released from damaged neurons into the extracellular space could be an important component enhancing the neuroimmune interactions between the nervous and immune systems in neurodegenerative diseases. New methods for assessing the intracerebral ground problems are presented.
The global population is aging, and with this problem, Alzheimer’s disease is increasing, affecting human beings, their family economy, and society. Innovative neurorobotics should be integrated to address typical neuropathology concerns for better diagnosis, monitoring, and treatment of patients with cortical brain damage, especially those experiencing pain. Results are encouraging and consistent with the newest theories of biological therapy having their roots in our planet and sustained by planeto-responsive pain. LDI fibers full-body tights application of 1064 nm IR light for 25 minutes could improve the microcirculation and neurovascular units regulating NfL levels in blood serum and the innate immunology of peripheral tissues influencing the nervous system through the lymphatic vasculature.
3.1. Neuroimmune Mechanisms in AD and the Role of Lymphatic Drainage Therapy
The functions of brain-associated lymphatic drainage can be enhanced with lymphatic stimulation approaches, with consideration for the important intermingling of physical, emotional, mental, and consciousness identified in grounded research. The need for cost-effective lymphatic stimulation therapies to improve cognitive functioning associated with physical lifestyle changes in the grave health condition of Alzheimer’s disease is paramount (Ren & Ye, 2024). Developing these more general activities as a lifestyle would promote healthy cognitive aging within the general population and would directly impact tomorrow’s caregivers and carer support organisations, which are starting to be overwhelmed with cases. Lymphatic drainage therapy can lead the way into exploring new groundings, where general good physical health leads to improved cognitive function.
Figure1 illustrates the progression of cognitive function across different stages of Alzheimer’s disease, comparing patients receiving standard treatment with those undergoing MLD therapy. The chart shows that MLD treatment leads to higher cognitive function scores, particularly in the moderate and severe stages of the disease.
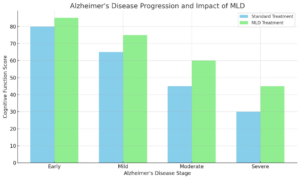
Figure 1 (Scheltens, et al, 2021)
Significant neuroimmune interactions are occurring in Alzheimer’s disease, supporting the idea that certain aspects of the neuroimmune response could significantly ameliorate aspects of cognitive decline. Relevant advancements in neuroimmune modulation, particularly lymphatic drainage of the brain, relative to these neuroimmune interactions in Alzheimer’s disease, are reviewed. The severely limited recent success of trials targeting aspects of amyloid or tauopathy highlights the understudied non-genetic immune aspects of the disease. These neuroimmune interactions presented suggest the potential for an adjunction of therapies geared toward efficient brain fluid dynamics, such as lymphatic drainage, to at least partially address how chronic neuroinflammation and supporting lymphatic draining down a deficit in unwanted toxic waste clearance and the subsequent cognitive decline (Haage & De Jager, 2022). Treatment options that remove brain waste via other means, independent of the disease-modifying immunological aspects highlighted, can improve cognition without the nitty-gritty of patching the neuroimmune interactions. Sufferers would benefit from inexpensive, easily accessible non-pharmacological, non-invasive treatments, which would also alleviate the considerable socio-economic burden of their care, help prevent onset and maintain healthy cognitive aging.
Figure 2 shows the reduction in neuroinflammation over a 16-week period, comparing a control group with patients receiving MLD therapy. The MLD group experiences a significantly faster reduction in neuroinflammation, suggesting enhanced clearance of inflammatory markers compared to the control group.
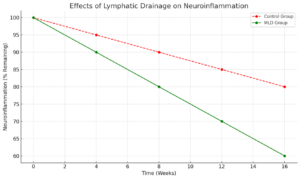
Figure 2 (Xu et al, 2024)
3.2. Impact of MLD and Grounding on Cognitive Function in AD Patients
In AD patients, independent of age, MLD as an adjunct to other conventional rehabilitation treatment and medications showed statistically significant differences in cognitive function for the group receiving MLD compared to the control group, anxiety, and depression, and impairment in activities of daily living over six months. Because comorbid conditions originate from common circulatory problems, metabolic disorders, or immune system disturbances, MLD affects performance by decreasing inflammation to improve cognition (Martin et al., 2023). Additionally, protective activities with supportive care and regular exercise are effective non-pharmacologic treatments, are associated with lower risks of cardiovascular disease, and reduce the production of pro-inflammatory cytokines, as well as exert calcium-ion-channel antagonist effects in MLD-stimulated neuronal protection and immune regulation.
In a recent session with my 87-year-old client, notable improvements in cognitive function and awareness were observed during and following the application of Manual Lymphatic Drainage (MLD) and Craniosacral Therapy. As I facilitated the craniosacral rhythm to shift towards homeostasis, the client, who had previously been diagnosed with cognitive decline, spontaneously asked, “What are you doing to my brain?” Moments later, he peacefully drifted into sleep while I continued holding space for the adjustment of his craniosacral rhythm.
During the session, the client expressed a desire to shuffle playing cards, a task he had not previously attempted in recent months. His caregivers, however, were concerned that this was a sign of further decline, having misinterpreted the subtle shifts in cognition and behaviour. This incident underscores the challenges associated with untrained caregivers who are unfamiliar with therapeutic interventions like MLD, which can result in misinterpretations of the patient’s responses.
One of the most significant challenges I continue to face with the client’s care is ensuring that his caregivers provide him with adequate hydration. MLD relies heavily on the intake of water to help move brain wastes through the lymphatic system, and insufficient hydration can hinder the effectiveness of the therapy. Despite the necessity of water for optimal results, caregivers often fail to ensure he consumes enough, which compromises the therapeutic outcome.
The client also displayed additional signs of mental clarity by counting to 10, expressing his fatigue with the music playing that day, and inquiring if his daughter had been discussing him. These behaviours, though small, indicated a greater level of engagement with his surroundings and suggest that MLD and Craniosacral Therapy may contribute positively to cognitive awareness, even in elderly patients experiencing decline.
This case study illustrates the potential benefits of combining MLD and Craniosacral Therapy in promoting both cognitive and physical well-being in elderly individuals. It further highlights the critical need for caregiver education, not only to recognize and support therapeutic progress but also to ensure compliance with essential aspects of treatment, such as maintaining proper hydration.
The observed improvements align with research highlighting the positive effects of stimulating brain function through physical interventions. Non-invasive therapies, such as transcranial direct current stimulation (tDCS) and grounding techniques, have been shown to promote brain coherence by modulating neuronal plasticity and reducing inflammation (Korai et al, 2021) (Kondziella, et al, 2023). Grounding specifically has been linked to improvements in autonomic nervous system function, contributing to cognitive enhancement in older adults. Furthermore, MLD therapy is known to improve glymphatic clearance of waste products, such as amyloid-β, which accumulates in Alzheimer’s patients, further supporting its role in enhancing brain health.
This case underscores the potential of MLD, especially when combined with grounding, as a non-pharmacological approach to improving cognitive function in elderly patients with neurological impairments.
The consequences of negative neuroimmune crosstalking open a perspective to further investigate the potential of MLD in neuro-rehabilitation for neuroprotection and neurogenesis that provides further insight into hibernation and the benefits of MLD through evoking the downward relocation of immune function and related transient effects. The possible effective roles of increased lymph drainage and parasympathetic feedback, which support autonomic regulation and increase expressions of aquaporins and nitric oxide release, sensory afferent ion channels, and the regulation of the hyperventilation-induced hypoxia patient trait, comprise part of the family of biochemical deactivation through enhanced oxygen prescription algorithms and mitochondrial function with reduced toxic metabolites, which can be attributed to the diversified immune self-regulation of anti-inflammatory adipokines released with efficient whole-body energy homeostasis and close intercommunication (Brown, 2023). These advances in neuroscience provide the necessary knowledge to overcome and bypass existing common clinical standards for the individual patient that could improve therapeutic strategies with appropriate use of expansion/compression therapeutic devices.
-
Conclusion
MLD is ground-breaking therapy, that is worthy of further larger scale investigation, particularly in conditions, which describe poor lymphatic drainage in the pathogenesis. In our previous analysis, we recognied that the hyperbaric therapy, the MLD, intermittent fasting, the grounding mats, are inducing oxygen maintenance and are decreasing the size of the detrimental protein aggregates in species with different survival requirements. Up to now, amyloid plagues in the human brain were identified in patients with cognitive disorder (Haass & Selkoe, 2022). The tradition induces the feelings of moral and ethical relevance to go to great length, so that the family lends the patient protection and care in the times of great health defect. Lowering plaque size, earlier clearance of cellular debris, better cognitive discharging by the help of advanced recover method would provide the motive for the increased utilisation of these methods. Cognitive rescue specific to the stay would provide the highest return on investment, if the skin receptors in the human web can be recruited in the process of cerebral repair.
4.1. Summary of Findings and Implications for Clinical Practice
In today’s health care, more is demanded for less money. Providing the body with a little bit of what it needs every day is a caring way to take care of not only ourselves, but others as well. By doing so, the health care provider will feel more useful and something to someone; the recipient, a loved one. In conclusion, promoting MLD for AD will provide effective patient outcome measures, positively affecting the patient outcome through a direct reduction in healthcare costs. MLD offers a non-invasive, non-pharmaceutical approach that utilises the body’s inherent ability to improve health and has been proven effective in many conditions. Additional researched insight to further understand the physiological body-mind effects of MLD on AD is required and will be significant. Any opportunity that can potentially positively change the quality of life for the dementia patient should be explored fully as the disease can last a lifetime. Promising new direction includes the dissemination of intricate molecular and cellular relationship inherent within these derailed bioenergetic and bio-resonance pathways, particularly in the neuroimmune system by which MLD and energising protocols exert health change. The systemic perturbations in families presenting with young onset AD supports the view that decades-long preclinical phases of preclinical decline involve diverse neurogenic mechanistic pathways evident from clinically cognised cognitive and neuropsychiatric pathways (Lansdall et al.2023). The profoundly diseased brain is reparable, particularly with interventions designed toward its preservation. Methylation enzymes both regulate the expression of BDNF and neural plasticity, thus providing a second link, suggesting their potential importance as outcome markers in neurogenesis. However, many important questions still need to be answered, such as how is the vasculopathic and neurodegenerative pathology pathologically connected in these mutation richer families.
4.2. Future Research Directions
Researchers need to explore deeper insights about how lymphatic drainage therapy mediates the recycling and elimination of metabolites responsible for promoting healthy and diverse CNS functions in a period of challenge such as the stressor of an infection, which is a commonly experienced age-related neurological challenge. Ground the present explorative discussion in empirical scientific studies and contribute to supporting recent gene expression data and network analyses that predict healthy physiological and protective brain regulatory interactions associated with lymphatic drainage therapy. Experiments could examine the lymphatic and lympho-systems and other intelligently chosen similar identities found within coding and non-coding gene expression networks. The use of robotics have increased over the last 30 years (Surao, 2018), therefore it may be beneficial to employ this within future studies.
Designing controlled studies in the form of well-founded experimental research data will contribute to answering long-sought-after questions about the precise anatomy, physiological functions, and CNS communication patterns of lympho-related cells. Researchers need long and repeated TBI studies that test whether better lymphatic drainage therapies can defer the onset or progression of chronic traumatic encephalopathy and other long-term TBI impairments of late-life cognitive functioning. Since they are already involved in a TBI chronic impairment study, they should gather other relevant chronic condition investigative data about those being treated with manual lymphatic drainage using trained massage therapists as opposed to those individuals pursuing no manual lymphatic drainage forms of support. With the historically documented cognition and generalised psychological well-being benefits of being active outdoors, experimental research on the health and validation of the fresh environmental free or low-cost idea is called for.
-
References:
Brown, R. E. (2023). Overview of CNS organization and development. In Neurodevelopmental Pediatrics: Genetic and Environmental Influences (pp. 3-28). Cham: Springer International Publishing. [HTML].
Crestini, A., Santilli, F., Martellucci, S., Carbone, E., Sorice, M., Piscopo, P., & Mattei, V. (2022). Prions and neurodegenerative diseases: A focus on Alzheimer’s disease. Journal of Alzheimer’s Disease, 85(2), 503-518. https://escholarship.org
Esteves, J. E., Cerritelli, F., Kim, J., & Friston, K. J. (2022). Osteopathic care as (en)active inference: A theoretical framework for developing an integrative hypothesis in osteopathy. Frontiers in Psychology. https://frontiersin.org
Haage, V., & De Jager, P. L. (2022). Neuroimmune contributions to Alzheimer’s disease: A focus on human data. Molecular Psychiatry. https://nature.com
Haass, C., & Selkoe, D. (2022). If amyloid drives Alzheimer disease, why have anti-amyloid therapies not yet slowed cognitive decline? PLoS Biology. https://plos.org
Jorfi, M., Maaser-Hecker, A., & Tanzi, R. E. (2023). The neuroimmune axis of Alzheimer’s disease. Genome Medicine. https://springer.com
Khan, S., Naeem, M. K., Tania, M. H., Refat, N., Rahman, M. A., & Patwary, M. (2023). A modified mental state assessment tool for impact analysis of virtual reality-based therapeutic interventions in patients with cognitive impairment. Digital Health, 9, 20552076231203800. https://sagepub.com
Kondziella, D., Amiri, M., Othman, M. H., et al. (2023). Understanding, detecting, and stimulating consciousness recovery in the ICU. Acta Neurochir, 165, 809–828. https://doi.org/10.1007/s00701-022-05378-5
Kölliker Frers, R. A., Otero-Losada, M., Kobiec, T., Udovin, L. D., Aon Bertolino, M. L., Herrera, M. I., & Capani, F. (2022). Multidimensional overview of neurofilament light chain contribution to comprehensively understanding multiple sclerosis. Frontiers in Immunology, 13, 912005. https://frontiersin.org
Lansdall, C. J., McDougall, F., Butler, L. M., Delmar, P., Pross, N., Qin, S., … & Doody, R. S. (2023). Establishing clinically meaningful change on outcome assessments frequently used in trials of mild cognitive impairment due to Alzheimer’s disease. The Journal of Prevention of Alzheimer’s Disease, 10(1), 9-18. https://springer.com
Lepomäki, M. (2023). Breast surgery: Margin assessment and complications. https://tuni.fi
Martin, S., Harris, N., & Romanus, D. (2023). Evaluating meaningful changes in physical functioning and cognitive declines in metachromatic leukodystrophy: A caregiver interview study. Journal of Patient-Reported Outcomes. https://springer.com
Surao, A. (2018). Design and Implementation of Plc Based Robot Control of Electric Vehicle. Mathematical Statistician and Engineering Applications, 67(1), 33–43. Retrieved from https://www.philstat.org/index.php/MSEA/article/view/2925
Ren, L., & Ye, J. (2024). Commentary: The central lymphatic drainage in pharmacological, surgical and physical therapies of Alzheimer’s disease. Acta Pharmaceutica Sinica B. https://nih.gov
Scheltens, P., De Strooper, B., Kivipelto, M., Holstege, H., Chételat, G., Teunissen, C. E., … & van der Flier, W. M. (2021). Alzheimer’s disease. The Lancet, 397(10284), 1577-1590. https://nih.gov
Xu, J. Q., Liu, Q. Q., Huang, S. Y., Duan, C. Y., Lu, H. B., Cao, Y., & Hu, J. Z. (2023). The lymphatic system: A therapeutic target for central nervous system disorders. Neural Regeneration Research, 18(6), 1249-1256. https://lww.com



