Research Objectives:
To provide an insight into conditions for implementing synchronous digital mental health interventions) in ‘real-world’ settings, thus contributing to the feld of implementation science.
Keywords:
Mental Health, Anxiety, Technology, Wellbeing
Bio
Prof. Dr. Parin Somani, Director of LOSD, is a distinguished Academic Scholar, TEDx Speaker, and Author, honoured the title of Mrs. Universe 2022 and crowned by Bollywood Actress Mahek Chahal. With 2 Academic and 6 Honorary Doctorates, she’s a multi-award-winner and humanitarian. She is a prolific author of 19 books, and a record-breaker recognised in Guinness World Records and multiple prestigious record books. She was invited to deliver a Keynote Speech at Harvard University, Cambridge University and many more. In her global travels to 127 countries, Prof. Dr. Parin Somani tirelessly contributes to education, women empowerment, and youth development.
Roxanne Boodhoo is an accomplished professional with a diverse and versatile background. Her extensive academic training has equipped her with a wide range of skills and knowledge, enabling her to excel in various roles. Roxanne is known for her strong work ethic, diligence, and commitment to undertaking any responsibilities assigned to her. She is deeply passionate about helping and supporting others, making her a compassionate and empathetic individual. Throughout her career, Roxanne has consistently demonstrated a dedication to making a positive impact, whether through her professional work or community involvement, striving to uplift those around her.
Abstract
Effective mental health promotion and prevention of mental disorders is an important social and economic goal. Anxiety disorders, depression, bipolar affective disorder, and schizophrenia are among the most common and burdensome mental disorders globally. One in four adults and one in ten young people suffer from one or more mental health disorders in Europe in any given year, and at least one in two will develop psychological distress during their lifetime. Even if mental health care capacities were to be dramatically increased, it would still be a challenge to reduce these figures. Given this context, efforts to promote good mental health and self-relaxation are gaining increasing importance. Policy-makers and health care provider alike see the potential of digital interventions to address these increasing needs and demands for mental well-being. Social isolation in the wake of COVID-19 has had adverse effects on mental health. Many people have turned to digital interventions to help them cope, often without much evidence on how effective these interventions are among different user groups and under different conditions. Social isolation due to the COVID-19 pandemic has had adverse effects on mental health. In response, many have turned to digital interventions with enthusiasm. Yet, enthusiasm alone is not enough: the individual and contextual factors that infuence the effectiveness of digital mental health interventions need to be better understood.
Introduction
Mental illnesses, including depression, anxiety, and post-traumatic stress disorder (PTSD), are a leading cause of global burden of diseases and economic loss, overshadowing other chronic medical illnesses (Saad et al., 2021). Within any given year, an estimated 26% of US adults, or about 1 in 4 individuals, are suffering from a mental illness. Only half of the people with a mental illness will seek help, and even if they are able to access care for behavioral health conditions, their treatment may not be evidence-based or guideline-concordant.
Therefore, there is growing pressure to find and implement evidence-based ways to combat the mental health crisis. One possible path to such evidence-based and scalable solutions might be through digital interventions, the use of technology to provide therapeutic support for mental illnesses. To provide affordable and accessible mental health interventions, there are several critical steps that stakeholders need to develop (Liu & Zhang, 2024). These solutions should be easy to use, scalable, and built using a bottom-up approach, with insights from the target users. Investigators working in collaboration with young mental health care users to develop user-centered digital tools allows for the expedited development of scalable options.
However, digital systems require incentive-based engagement and often function within complex systems characterised by public and digital architectures with competing goals. Whereas passive interventions, like educational websites, are appealing and non-invasive, but ignorable, while active, non-invasive digital interventions, like a mobile app installed on a user’s personal device, are disruptive and require high user participation. However, this also results in a demand on the user, a barrier to help-seeking, as users often need time to trust the system and assess the potential benefits.
According to the National Health Service almost 1 in 6 people in the last week encounter a common mental health issue like stress, decay, anxiety, or mental ill-health at the workplace. A daily stressor is the major symptom of difficulty in focusing and improving the patient’s well-being. If issues of well-being are not properly dealt early, they could lead to more serious mental health issues. If significant well-being treatment is offered, individuals with common mental health disorders gain from enhanced productivity and improved working and caring performance. Depression, anxiety, and insomnia are essential components of a major depressive disorder (Woodward et al., 2019). Therefore, well-being is not only an optimistic way to measure our life quality but deficiencies in well-being and illness may be a significant problem that creates factors that contribute to significant depressive and anxious problems and is also associated with numerous physical diseases. Nonetheless, it was revealed that training in mindfulness targeting anxiety showed significant changes of satisfaction with life.
The unprecedented challenges of a growing mental health crisis, exemplifed by the COVID-19 pandemic and its association with increases in mental health disorders, propelled the expansion of electronic interventions. These electronic interventions range from web-based and smartphone-based schedules to fully automated digital characters (avatars). Although there are proven efficient interventions and useful therapy delivery modes, these technological interventions have not been broadly implemented due to the demanding technological infrastructure and regular post-development research to guarantee effectiveness, as well as adherence to local mental health care regulations (Mohammed, 2023).
E-mental health interventions may implement methodologies dependent on digital components to identify and monitor mental illness tendencies, to avoid and detoxify emotional distress, to care of present mild psychiatric conditions, to support mental health disorders as a complementary approach to a weaker central therapy, or to avoid decompensating the chronic and acute psychiatric disorders with routine maintenance treatment by the acceptable mix of both digital and face-to-face therapy techniques. Therefore, it is important in this modern era to advance communications with mental health care centers to make modifications in the present psychotherapeutic interventions to develop additional ethnic treatment packages, and also to develop innovative e-therapy systems, with particular emphasis on how to envelop and monitor them in regular health practices and all that efficiently, appropriately, and ethically through the integration of tested, proof based treatment methodologies, in addition to the flexible contribution of new clinical knowledge from every current delivery form, thereby increasing the overall impact (Robinson et al., 2023).
Increasingly, agencies are looking beyond face-to-face singular treatments towards digital solutions. National Health Service (NHS) England have established the ‘Digital First’ initiative, aiming to expand digital services as a cost-effective and inherently patient-centred option for service users to access support (Easton et al., 2021). Since 2016, NHS England has aimed to increase digital services to England, with over 58 services now available. If digital solutions to reduce the demand for face-to-face services are provided centrally, the service may see need fewer appointments. Such interventions may also improve patient-clinician communication, with attractive proposals of eHealth records (EHRs).
Writing Health applications are helping to reshape the way we think about mental health treatment (Woodward et al., 2019). A change in patient expectation and the promotion of self-management in health services is tangible evidence of the effect of not only interventions in mental healthcare, but also digital and mobile technologies that have a major part to play in promoting mental well-being and accessing interventions (A. J. De Witte et al., 2021). Mobile technologies have been identified as superior for delivering such treatment or interventions for many reasons. The results from this review will be able to help users choose an effective smartphone application to improve their psychological health according to the systematic evaluation of free and fee-based smartphone applications (Santhanam et al., 2023). The issues of needing external development funding and content updating were evaluated as suboptimal. Even multiform interventions to create less professional dependence on one of the counter participants in the user-interview process were indicated. For an advanced updating of counteractive smartphone applications in an ethical and moral manner, researchers should collaborate closely with development and production units. Mobile mental health apps have seen rapid and robust development, shaping the epidemiology of mental health services (Koh et al., 2022). The increasing prevalence of mental health produces a challenging and diversified usage of such mobile applications, which need to be continuously reviewed. This study aimed to systematically review and rate smartphone applications to reduce alcohol consumption and depressive symptoms among youth (Magwood et al., 2022). The umbrella review was conducted using several databases, such as PubMed, ScienceDirect, Cumulative Index to Nursing and Allied Health Literature, and Google Scholar. Keywords in the umbrella review were: (1) mobile apps, (2) youth, (3) depression, (4) alcohol addiction, (5) randomized controlled trials or quasi-experimental trials, and (6) pre-post comparison studies.
The quality of the included studies in the umbrella review was assessed using relevant tools for systematic reviews and meta-analyses of randomized controlled studies, and the results were presented using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Literature Review
Third Generation Cognitive Behavioral Therapy (CBT) has garnered empirical support in treating various mental health concerns with good effect sizes. Thus, third generation CBT is regarded as the state-of the-art psychological therapy. When applying third wave CBT models, very few researchers or therapists use manualized third wave CBT treatments, in contrast to manualized CBT.
This suggests that a more adaptive, flexible, and holistic approach to understanding what specific persons want a change in is needed. Third wave CBT focuses on understanding mental challenges with a more functional perspective, emphasizing factors such as personal values, and targets experiential avoidance and psychological inflexibility in addition to matching selected strategies to actual functions of the specific mental challenge. Hence, the future of personalized third wave CBT can potentially be digital and machine learning can be used to achieve psychological personalized treatments, according to the user’s profile (Zhao et al., 2024).
Most people experience mental health challenges at some point in their lives. Modern challenges, including COVID-19, have made the demand for effective and scalable digital mental health interventions ever more salient (Somani, P., 2020). The shift to remote mental health care has accelerated the development of innovative digital mental health interventions, including those that harness machine learning techniques.
However, for these interventions to be effective, they must be grounded in a deep understanding of psychological processes and evidence-based therapies. The tension between the potential flexibility of digital interventions and the need for clear and standardized interventions from a clinical perspective will be discussed (Sage Chen et al., 2022). Digital mental health interventions have the potential to transformatively improve mental health care in ways that are likely to be unprecedented. This new and emerging field of mental health interventions primarily involves providing mental health services or self-help services via web portals, online counselling, secure e-mailing, video calls, chat rooms, health-related apps, or automated text messages. Sometimes, monitoring or interventions can be integrated in mobile interventions. Other intervention forms can contain augmented or virtual reality. Advanced interventions include decision and prediction functionalities. Digital mental health interventions can be preventive or therapeutic. They can range from education and promotion to destinations such as crisis intervention and assessment and therapy services. These therapies can represent different schools of psychotherapy, including cognitive-behavioral therapy, dialectic behavior therapy and mindfulness-based interventions. Moreover, therapies can be provided by different stakeholders such as health care professionals and clinicians to digital agents based on different machine-learning approaches. Virtually any mental disorder or symptom can be the target and any form of digitally mediated interaction between people or digital artifacts related to mental health are eligible. Topos of digital mental health interventions can span mental health literacy, wellbeing and self-help, psychoeducation, preventing, diagnosis, therapy and monitoring or assessment (Jadhakhan et al., 2022).
Mental health conditions are among the most common and widespread morbidities worldwide (Mohammed, 2023). Digital mental health services, provided through the use of mobile technologies or media, have gained increased attention and momentum in mental health care contexts, leading to significant changes in the therapeutic landscape. Mental health conditions have been long associated with social and economic costs. Further, these morbidities are associated with a higher risk of comorbidities or chronic health conditions. Moreover, with the COVID-19 pandemic, rates of mental health illness and psychological distress might have increased exponentially. It is therefore critical for societies to invest in strategies that prevent mental health conditions or reduce their effects. Researchers studying the mental health of people with chronic diseases have reported that people with a chronic disease have twice the risk of depression compared with the general population. Given that mental conditions might have a bidirectional association with physical conditions, preventing or managing mental health conditions early-on could support the prevention, amelioration or management of chronic health conditions as well. This prevention and early intervention might help in reducing wider societal implications throughout the lifespan of individuals.
Results and Discussion
Digital health care interventions such as smart phone -based apps aimed at mental health promotion are widely used, few systematic reviews have been published providing an overview of what is available. However, recently published work, primarily focused on low-cost mobile apps and web-based platforms, has nonetheless identified advancements in this area. Smartphone applications (apps) have been developed, for example, to monitor and treat mood disorders such as depression. These apps have been shown to significantly reduce self-reported depression symptoms. Limitations include the relatively small number of mental health disorders targeted by available apps and approaches mainly anchored in the principles of cognitive-behavioral therapy.
In another systematic review, Firth et al (2017) identified a substantial gap in apps tailored to address mental well-being proactively as opposed to providing treatment for existing symptoms. Notwithstanding these limitations, digital selfhelp interventions are recognized as having great potential for scalability and cost-effectiveness for population-level public mental health. Such adaptive digital health inter3. Results and Discussion venations suitable for broad mental well-being promotion are essential in the current scenario. Rooted in optimal human-computer interaction, they can provide real-time objective measures and timely, personalized support to the user for different contexts. There is ongoing scaling-up of the development of digital apps from a passive monitoring role primarily in the mental health/illness places to also include those that aim at addressing mental well-being and relaxation through reminders and live sessions in nonclinical and nonstandard settings (Saleem et al., 2021).
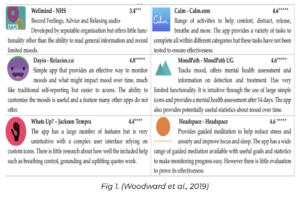
A number of digital interventions including smartphone applications (apps), wearable devices, and web-based platforms have been developed to address mental health challenges. Substantial progress has been made in the development and evaluation of digital interventions to provide real-time support, monitor symptoms, promote relaxation and enhance mindfulness (Woodward et al., 2019). The use of digital technologies for psychological interventions has been discussed extensively. In a systematic review by Firth et al (2017), apps targeting depression and/or anxiety showed greater effect sizes at postintervention than those targeting mental well-being. In a 2017 meta-analysis of 18 studies involving university students, Carey et al found a significant effect size (g=.25) for psychological intervention with mobile apps relative to waiting list control. Digital interventions for mental health include a wide range of technologies—mobile devices and wearable devices—and methods for monitoring and enhancing mental well-being such as gaming and 3D visualisation. Technologies are available for real-time monitoring of well-being with multiple indices (eg, psychophysiological, movement, and movement patterns), positive feedback, and automated (‘smart’) guidance. Smartphone and wearable devices make the collection of physiological data cost-effective and convenient. Figure 1 highlights a summary of the most popular mental health apps on the Google Play Store compared to Wellmind, an app developed by the NHS.
A growing area of research called “digital health” is aimed at understanding how technology and digital tools can be used to improve health outcomes in patients with a variety of diseases. For example, a recent review identified a reliance on stand-alone products rather than ecosystem integration (i.e., how an app contributes to the broader collection of mental health tools), proprietary systems (i.e., apps and digital health products created by one company rather than supporting interoperability with other tools), and an underrepresentation of apps focused on anxiety (Romael Haque & Rubya, 2022). If users do not continue to engage with interventions (i.e., repeated use or longer usage periods), it is unlikely that outcomes will be achieved. Several psychological theories have been developed to explain the process of why individuals continue to engage with systems and how to influence them. Digital interventions for mental health promotion continue to increase in prevalence as a way to overcome several of the barriers to mental health care (e.g., lack of resources, physical and social accessibility; (Fonseca Zuccolo et al., 2021)). Moreover, digital interventions offer completions in an innovative way that can include more tailored and real-time support. However, user engagement with digital interventions for mental health continues to be a challenge. Engaging and retaining users alternate digital interventions can promote the utilization of services, and potentially improve health outcomes and well-being ( (Saleem et al., 2021)).
Supportive strategies like reminders, gamification, and push notifications have been successful in increasing engagement with digital interventions. A digital mental health intervention that enhanced their implementation of key engagement components was able to increase the number of completed activities by over 20% compared to their standard implementation.
Proposed strategies will need to be assessed further in empirical studies in order to evaluate the benefits and risks associated with different engagement strategies.
Conclusion
Capturing the voices of service beneficiaries is crucial to developing and improving mental health services. Many service users have now experienced the recent digital turn in mental health; less is known about their experiences and needs. This study aimed to understand service users’ attitudes and experiences of accessing and engaging with digital mental health interventions, comparing these with their experiences of traditional face-to-face services. A meta-ethnographic synthesis was conducted of qualitative research comparing service users’ experiences of accessing digital interventions and traditional face-to-face mental healthcare. Included studies were those published in English about digital mental health interventions and their effectiveness on common mental disorders (CMD) in primary care. Outcomes were changes in mental health symptom severity and experts’ perspectives on implementation of digital mental health interventions. Metadata and a quality assessment of the quantitative studies were conducted. 14 quantitative studies were included with data (n > 1000). Interventions were seen as acceptable. Effects were suggested to be dependent on course and symptom severity. Digital mental health interventions require tailored, ethical and evidence-based implementation. Utilization of digital health should be naïve and encouraged to benefit people.
The COVID-19 pandemic has been particularly threatening for the mental health of many people, with increased levels of mental distress and spiking mental health problems in certain populations (Mohammed, 2023) (Hanf et al., 2021). This situation has given a push for the development and implementation of (digital) (preventive) mental health care. Although digital interventions can bring many benefits in facilitating timely, personalized and remote support, we must be aware of potential negative side effects of digital mental health solutions.
This editorial reflects on the experiences of digital mental health interventions in the first year of the COVID-19 pandemic, mainly from ongoing research programs in Specialized Mental Health Care in Dutch treatment programs. In these digital interventions we address both people with and without current mental health problems. Furthermore, digital mental health interventions are integrated in routine mental health care programs. From these experiences, we have learned a few lessons, and make recommendations to guide future implementation and development of digital mental health interventions beyond this COVID-19 period. With these recommendations we aim at avoiding stigmatization and dismantling barriers to equitable and ethical digital mental interventions. And in this way maximizing the effectiveness and applicability of digital mental health interventions for everybody.
Artifcial Intelligence therapies have been shown to have a positive impact on depression and anxiety. Wearable devices have the potential to collect continuous cardio data in the real world, which can be integrated with momentary self-report data and ecological momentary assessments for more fine-grained tailoring of (intervention) components. Most literature addressing mental health and technology is very clinical: we question whether technological solutions have to be large-scale and institutionalized, or can there be sand-boxed (prototype) or community-based solutions next to larger platforms. We would advocate that in technological design, for every problem, about as many types of solutions can also exist. The importance of having a variety of technological solutions could be to accommodate (in)formality, but also a one-size-fts-all approach may not work for all users different populations, age groups. Technological challenges in creating digital interventions for mental well-being (Gu et al., 2019). Digital and mobile interventions have demonstrated success with respect to a range of app-based and web-based interventions, others have looked at text message interventions or other types of digital interventions like sensors and smart devices. The efficacy of such interventions is also shown to depend on different factors, and understanding which digital interventions or settings are most successful is important to disseminate successful interventions.
References
A. J. De Witte, N., Joris, S., Van Assche, E., & Van Daele, T. (2021). Technological and Digital Interventions for Mental Health and Wellbeing: An Overview of Systematic Reviews. ncbi.nlm.nih.gov
Blease, C., Locher, C., Leon-Carlyle, M., & Murali Doraiswamy, P. (2019). Artifcial Intelligence and the Future of Psychiatry: Qualitative Findings from a Global Physician Survey. [PDF]
Easton, K., Kellett, S., Cooper, M., Millings, A., Varela, J., & Parry, G. (2021). Blending Cognitive Analytic Therapy With a Digital Support Tool: Mixed Methods Study Involving a User-Centered Design of a Prototype App. ncbi.nlm.nih.gov
Fonseca Zuccolo, P., O. Xavier, M., Matijasevich, A., Polanczyk, G., & Fatori, D. (2021). A smartphone-assisted brief online cognitive-behavioral intervention for pregnant women with depression: a study protocol of a randomized controlled trial. ncbi.nlm.nih.gov
Gu, J., Du, C., & Zuo, W. (2019). Galactic Stellar Populations from Photometric Metallicity Distribution Functions. [PDF]
Hanf, M., Hirt, J., & van den Akker, M. (2021). Primary care professionals’ attitudes towards digital health interventions for common mental disorders: study protocol for a mixed methods systematic review. ncbi.nlm.nih.gov
Jadhakhan, F., Blake, H., Hett, D., & Marwaha, S. (2022). Effcacy of digital technologies aimed at enhancing emotion regulation skills: Literature review. ncbi.nlm.nih.gov
Koh, J., Y. Q. Tng, G., & Hartanto, A. (2022). Potential and Pitfalls of Mobile Mental Health Apps in Traditional Treatment: An Umbrella Review. ncbi.nlm. nih.gov
Liu, J. & Zhang, Y. (2024). Understanding and Facilitating Mental Health Help-Seeking of Young Adults: A Socio-technical Ecosystem Framework. [PDF]
Magwood, O., Saad, A., Ranger, D., Volpini, K., Rukikamirera, F., Haridas, R., Sayf, S., Alexander, J., Tan, Y., Petkovic, J., & Pottie, K. (2022). PROTOCOL: Mobile apps to reduce depressive symptoms and alcohol use in youth: A systematic review and meta‐analysis. ncbi.nlm.nih.gov
Mohammed, H. (2023). Technology in Association With Mental Health: Meta-ethnography. [PDF]
Robinson, N., Connolly, J., Suddrey, G., & J. Kavanagh, D. (2023). A Brief Wellbeing Training Session Delivered by a Humanoid Social Robot: A Pilot Randomized Controlled Trial. [PDF]
Romael Haque, M. D. & Rubya, S. (2022). For an App Supposed to Make Its Users Feel Better, It Sure is a Joke — An Analysis of User Reviews of Mobile Mental Health Applications. [PDF]
Rukn al-Din, R. (2020).Advancing psychosocial measures for COVID-19 affected populations: Perspectives on digital health interventions promoting health equity. osf.io
Saad, A., Bruno, D., Camara, B., D’Agostino, J., & Bolea-Alamanac, B. (2021). Self-directed Technology-Based Therapeutic Methods for Adult Patients Receiving Mental Health Services: Systematic Review. ncbi. nlm.nih.gov
Sage Chen, Z., Prathamesh, undefned, Kulkarni, undefned, R. Galatzer-Levy, I., Bigio, B., Nasca, C., & Zhang, Y. (2022). Modern Views of Machine Learning for Precision Psychiatry. [PDF]
Saleem, M., Kühne, L., Karolina De Santis, K., Christianson, L., Brand, T., & Busse, H. (2021). Understanding Engagement Strategies in Digital Interventions for Mental Health Promotion: Scoping Review. ncbi. nlm.nih.gov
Santhanam, S., P, K., MS, B., & Kumar Rajagopal, M. (2023). Amity — A Hybrid Mental Health Application. [PDF]
Somani, P. (2020). The Impact of COVID-19 on Human Psychology. In B. S. Lal, & N. Patel, Economics of Covid-19 Digital Health Education & Psychology (pp. 328-357). New Delhi: Adhyayan Publishers & Distributors.
Villarreal-Zegarra, D., A Alarcon-Ruiz, C., Melendez-Torres, G. J., Torres-Puente, R., Navarro-Flores, A., Cavero, V., Ambrosio-Melgarejo, J., Rojas-Vargas, J., Almeida, G.,
Albitres-Flores, L., B Romero-Cabrera, A., & Huarcaya-Victoria, J. (2022). Development of a Framework for the Implementation of Synchronous Digital Mental Health: Realist Synthesis of Systematic Reviews. ncbi.nlm. nih.gov
Woodward, K., Kanjo, E., & Brown, D. (2019). Challenges of Designing and Developing Tangible Interfaces for Mental Well-being. [PDF]
Woodward, K., Kanjo, E., Brown, D., M. McGinnity, T., Inkster, B., J Macintyre, D., & Tsanas, A. (2019). Beyond Mobile Apps: A Survey of Technologies for Mental Well-being. [PDF]
Zhao, Y., Li, T., & Sobolev, M. (2024). Digital Wellbeing Redefned: Toward User-Centric Approach for Positive Social Media Engagement. [PDF]




